
The SDoH and Health Equity Connection
As we wrap up the Social Determinants of Health (SDoH) series, we circle back to how this data can ultimately impact health equity. Throughout out the series, we’ve discussed how nursing can impact SDoH data, the guidance by CMS and other agencies on the capturing of SDoH data, the importance of the standardization of that data for interoperability, and ultimately ensuring we are connecting patients to the appropriate community resources based on the SDoH needs identified.
For individuals to achieve optimal health, we need to consider all aspects that influence health. We can diagnose and develop treatment plans for patients, but if they don’t have a way to follow through on those treatments due to various economic or social factors, we won’t see improvements. The US Department of Health and Human Services (HHS) approved the Healthy People 2030 framework in 2018 with the vision of “A society in which all people can achieve their full potential for health and well-being across the lifespan.” (Healthy People 2030 Framework - Healthy People 2030 | health.gov) One of Healthy People 2030’s five overarching goals is specifically related to SDOH: “Create social, physical, and economic environments that promote attaining the full potential for health and well-being for all.”
Case Study: The Connection in Action
An exemplary case of connection in action comes from Houston Methodist, nursing informatics facilitated an effort where nurses gather SDoH data upon admission to the hospital using CMS recommended questions in five domains (food, housing, transportation, utilities, personal safety). They were then able to connect those patients needing resources to various community organizations through the facilities social workers. In addition, they were able to establish partnerships with some of those community organizations to send electronic referrals and receive electronic updates on how the needs were met back into the EHR, closing the loop. Initial data from a month across 9 hospitals in the greater Houston area revealed that, on average 20% of patients screened had positive responses for concerns in at least one domain. This demonstrates the importance of understanding these barriers for achieving improved outcomes. As more organizations move forward with obtaining and acting on SDoH data, it will be exciting to see the impact on patient outcomes.
Sharing SDoH Data for Large Scale Change
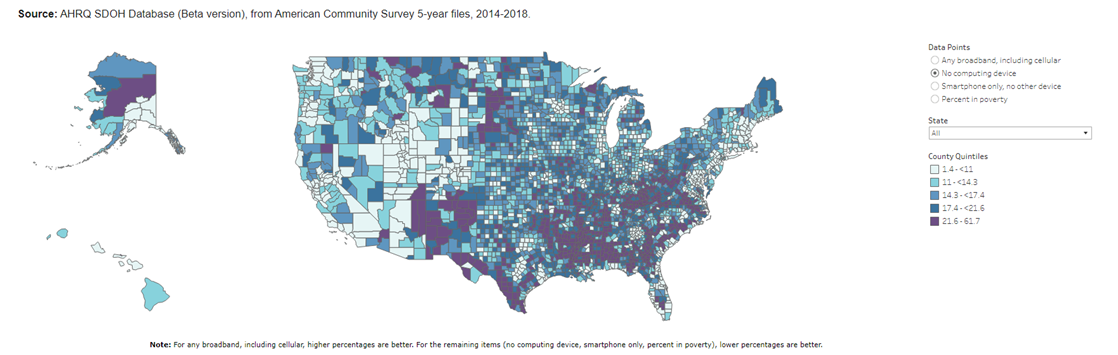
Additionally, as the data availability for SDoH increases on a larger scale, the better understanding we will have of the gaps in current resources on a national and even global scale. The NIH (Common Data Elements and Social Determinants of Health | Data Science at NIH), along with others, are working to use common data elements to collect consistent information that researchers can use to determine how SDoH contributes to health inequities. Using this data, they can demonstrate disadvantaged populations. One such example from AHRQ (Figure 1 -Social Determinants of Health Database | Agency for Healthcare Research and Quality (ahrq.gov)) shows areas within the United States where there were over 20% of households that had no computing device, including a smartphone/device. This information is critical with the growth of opportunities like virtual healthcare and determining how those households can have access to this rapidly rising healthcare option. For example, these specific communities may need to look at ways to send patients home with devices and ensure they have internet capability to be successfully monitored remotely and see improved outcomes. Continuing to gather and share this data on a global level has tremendous potential to advance health equity.
In Conclusion
This 5-part series on SDOH offers valuable insights around the why and how to implement a SDoH program at your healthcare organization. Engaging nursing and informatics is a great first step to developing a comprehensive model that effectively collects and shares data. Providing ways to seamlessly collect and share this data across the care continuum is the best way to ensure patients in your community are being connected to the resources they need. In addition, using standardized data elements to share SDoH data more broadly will help to improve health equity on a more global scale. Understanding and acting on SdoH is not only a step towards enhancing patient outcomes, but it is a crucial pathway to achieving health on a broader scale. As we navigate the intricate landscape of social determinants, we pave the way for future disparities are minimized, and well-being is accessible to all.
Figure 1
References
- Office of Disease Prevention and Health Promotion, Office of the Assistant Secretary for Health, Office of the Secretary, U.S. Department of Health and Human Services. Healthy People 2030 Framework - Healthy People 2030 | health.gov, accessed 12/7/23.
- U.S Department of Health and Human Services, last reviewed 4/11/23. Common Data Elements and Social Determinants of Health | Data Science at NIH, accessed 12/5/23.
- Figure 1: Social Determinants of Health Database | Agency for Healthcare Research and Quality (ahrq.gov)



